Research
Skip To:
Skip To:
A Singular Focus on Innate Immunity
The majority of advances in immunotherapy have focused on targeting the adaptive immune system; however, many patients do not respond to treatment, others lose responsiveness, and some diseases still entirely lack adequate therapy, leaving great unmet medical need. Furthermore, since adaptive immune system pathways are powerful and common to most pathogen responses, targeting them can carry the risk of systemic immune suppression or adverse immune activation.
In contrast, IFM Therapeutics is focused on developing drugs that target the innate immune system, the body's first line of immunological response and the master regulator of subsequent immune activity.
Driven By Advancements in Immune Science
Recent advances in the understanding of innate immune biology have demonstrated that the innate immune system is an underlying driver of many inflammatory and autoimmune diseases and is required to sustain chronic inflammation and autoimmunity throughout the course of disease. There is powerful human genetic evidence that ties particular innate immune sensors to both rare and common human diseases.
These data point to a multitude of potential drug targets and pathways across several therapeutic areas that offer a surgical strike on underlying disease drivers. Human genetics offers a rational path to identifying those patients most likely to respond to a particular therapy, bringing the potential for precision immunology to the fore.
On the flip side, cancers have evolved many ways to evade the immune system. The innate immune system is a key to engaging and activating the adaptive immune system to recognize and destroy a tumor, and IFM Therapeutics is pursuing mechanisms that allow the innate immune system to break tolerance, engage the adaptive immune system and synergize with immune checkpoint inhibitors.
From reducing overactivity in inflammatory disorders to stimulating activity to target cancer, we are only beginning to tap the potential of the innate immune system.
Adaptive vs Innate Immunity

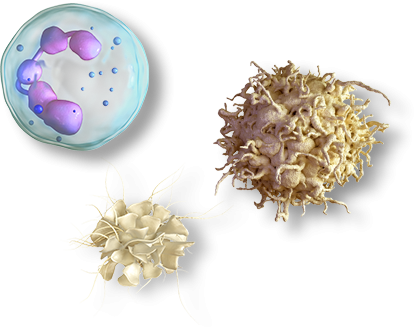
The adaptive, or acquired, immune system, is engaged by the innate immune system to supplement and magnify the immune system’s response to threats, but these adaptive responses are slow in onset and typically take more than a week to become fully active.
WATCH: How the Innate and Adaptive Immune Systems Work
Role of Innate Immunity in Major Disease Targets
Innate immune
responses are reduced
BODY STOPS
ATTACKING ITSELF
Innate immune
responses are enhanced
BODY ATTACKS
CANCER CELLS
Inflammatory Diseases
Advances in human genetics have taught us that many diseases are caused by inappropriate triggering of the innate immune system (also called sterile inflammation). This can lead to an excessive immune response and inflammation that can become chronic, driving a variety of autoimmune and auto-inflammatory conditions. Sterile activation of innate immune mechanisms drives inflammatory disease flares and chronic tissue damage and can lead to and sustain autoimmunity.
Cancer
The innate immune system is responsible for detecting cancer cells and signaling to the adaptive immune system for the destruction of tumors. But tumors can evolve to evade detection and avoid activating the innate and adaptive immune system. Paradoxically, it has also recently become clear that, in certain tumor contexts, chronic, low-level stimulation of the innate immune system can actually lead to immune suppression and immune evasion (a concept previously demonstrated in chronic viral infections). Understanding which mechanisms are operative in which tumors can guide the decision whether to activate or block a particular innate immune pathway to restore proper sensing of tumors and thus lead to new therapies for cancer.
Deep Dive into Innate Immunity
Surface Pattern Recognition Receptors (PPR)
- This type of PPR identifies external threats by pathogen-associated molecular patterns (PAMPs)
- Surface PPRs include toll-like receptors (TLR) and C-type lectin receptors (CLR)
Internal Pattern Recognition Receptors (PPR)
- This type of PPR identifies internal threat by PAMPS and damage-associated molecular patterns (DAMPs)
- Internal PPRs include some TLRs, NOD-like receptors (NLR) and RIG-I-like receptors (RLR)

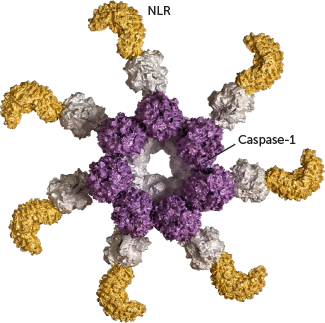
Inflammasomes
- After recognition of a PAMP or DAMP, some NLRs can change their shape to build a multi-protein structure known as an inflammasome
- Inflammasomes activate inflammatory processes, including pyroptosis, an inflammatory programmed cell death triggered by activation of caspase-1
- Pyroptosis can attract other immune cells to the site of activation
WATCH: How Inflammasomes Drive Inflammation
Research Publications
cGAS/STING
cGAS in action: Expanding roles in immunity and inflammation.A. Ablasser and Z.J. Chen
Science
March 2019
cGAS/STING
Parkin and PINK1 mitigate STING-induced inflammation.D.A. Sliter, R.J. Youle et al.
Nature
September 2018
cGAS/STING
Targeting STING with covalent small-molecule inhibitors.S.M. Haag, A. Ablasser et al.
Nature
July 2018
cGAS/STING
Oxidative damage of DNA confers resistance to cytosolic nuclease TREX1 degradation and potentiates STING-dependent immune sensing.N. Gehrke, W. Barchet et al.
Immunity
September 2013
AIM2
The DNA-sensing AIM2 inflammasome controls radiation-induced cell death and tissue injuryB. Hu, R.A. Flavell et al.
Science
November 2016
AIM2
Inflammasome-independent role of AIM2 in suppressing colon tumorigenesis via DNA-PK and AktJ.E. Wilson, J.P. Ting et al.
Nature Medicine
August 2015
Our Pipeline
IFM Therapeutics is developing drug candidates
that have the potential to overcome current clinical challenges in inflammation, autoimmunity, fibrosis, neuroinflammation and immuno-oncology.